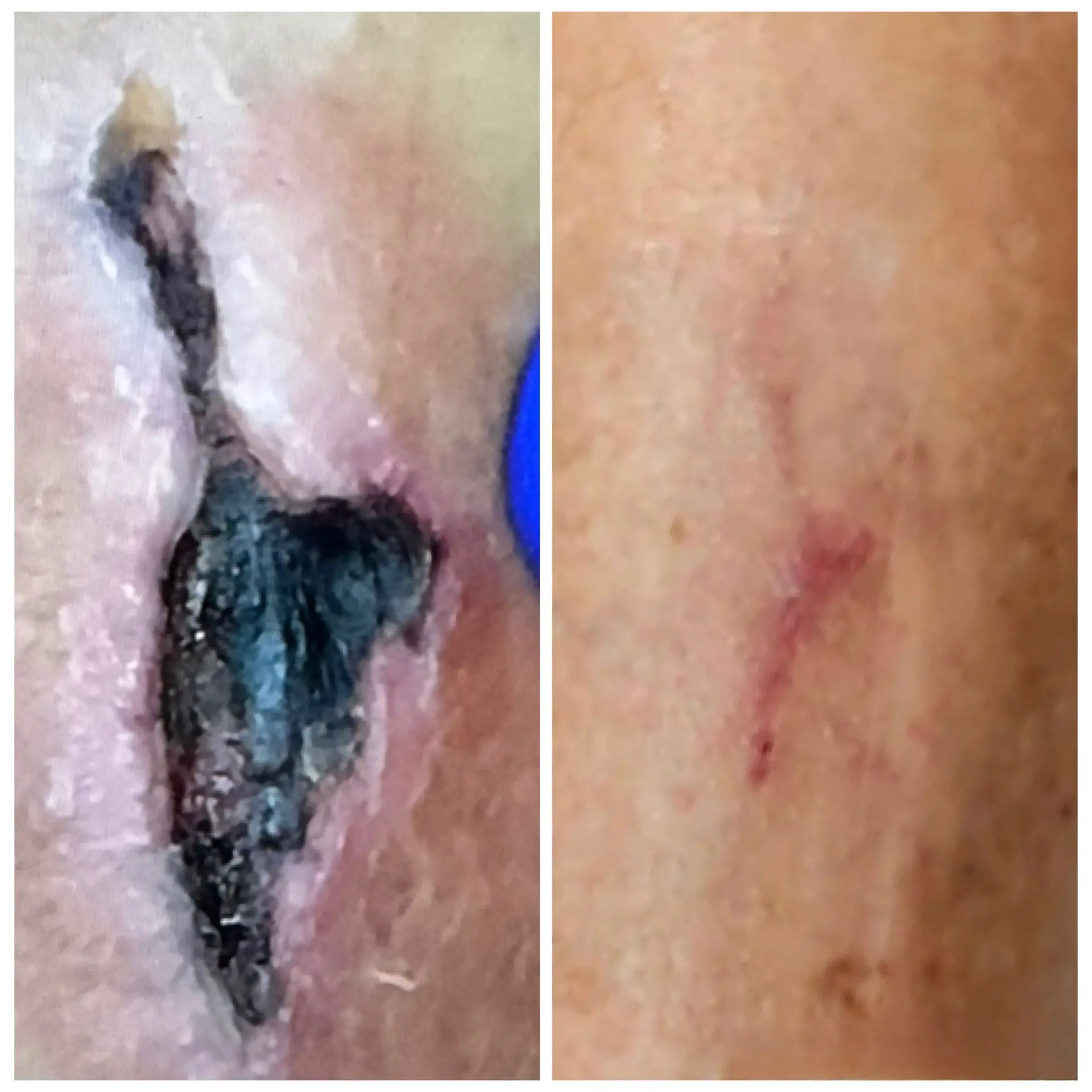
If you’re dealing with a wound that won’t heal, especially if you have a condition like diabetes, thyroid issues, or adrenal disorders, you need care that understands the root cause. Our endocrinology expertise sets our wound care apart. We don’t just treat the surface; we manage the underlying hormonal imbalances that are slowing your recovery.